Introduction
Monoclonal antibody drugs have emerged as powerful tools in the fight against cancer, revolutionising treatment approaches. These highly targeted therapies, developed through hybridoma technology, have significantly improved precision medicine and immune-based treatments. By specifically recognising and binding to cancer cells, monoclonal antibodies minimise damage to healthy cells, reducing side effects compared to traditional chemotherapy. Their success in treating various types of cancer, such as HER2-positive breast cancer and melanoma, highlights their potential. Ongoing research and advancements in engineering techniques offer promising prospects for the future, expanding the possibilities and effectiveness of monoclonal antibody drugs in combating cancer.
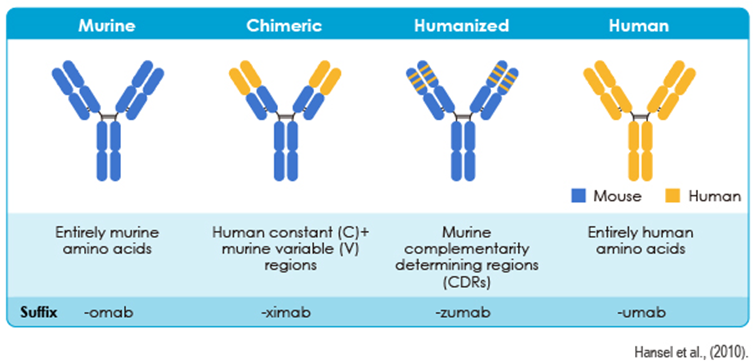
Types of Monoclonal Antibody Drugs
Mechanisms of Action
Monoclonal antibody drugs are designed to function in different ways. The mechanisms of action include:
1. Binding to specific cancer cell receptors
Monoclonal antibody drugs can be designed to bind to receptors that are overexpressed on the surface of cancer cells. By attaching to these receptors, the antibodies can interfere with crucial signalling pathways, inhibiting tumour growth or triggering cell death.
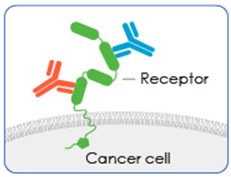
Example:
Trastuzumab (Herceptin®): Binds to the HER2 receptor on breast cancer cells, inhibiting tumour growth. It is used for HER2-positive breast cancer.
2. Antibody-dependent cellular cytotoxicity (ADCC)
Monoclonal antibody drugs can recruit immune cells, such as natural killer (NK) cells, to recognise and destroy cancer cells. The antibodies bind to cancer cells, while the immune cells recognise the antibody-bound cancer cells as targets for destruction.
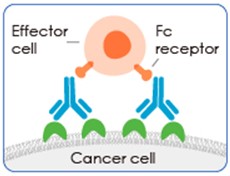
Example:
Rituximab (Rituxan®): Targets CD20, a protein found on B-cell lymphomas. It recruits immune cells for the destruction of cancer cells. It is used for non-Hodgkin lymphoma and chronic lymphocytic leukaemia.
3. Complement-dependent cytotoxicity (CDC)
Monoclonal antibody drugs can activate the complement system, a part of the immune system that triggers a cascade of reactions leading to the destruction of cancer cells. This mechanism enhances the immune response against tumours.
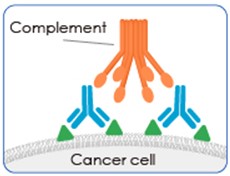
Example:
Ofatumumab (Arzerra®): Binds to CD20 on B-cell lymphomas, triggering complement-mediated cytotoxicity. It is used for chronic lymphocytic leukaemia.
4. Immune checkpoint inhibition
Some Monoclonal antibody drugs act as immune checkpoint inhibitors, blocking proteins that regulate the immune response, such as PD-1 or CTLA-4. By inhibiting these checkpoints, the antibodies unleash the body’s immune system, enabling it to recognise and attack cancer cells more effectively.
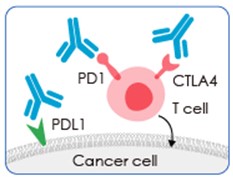
Example:
Pembrolizumab (Keytruda®): Blocks the PD-1 receptor on immune cells, enhancing the immune response against cancer cells. It is used for various cancers, including melanoma, lung cancer, and head and neck cancer.
5. Anti-angiogenesis
Monoclonal antibody drugs can inhibit the formation of new blood vessels that supply nutrients to tumours. By targeting and blocking specific molecules involved in angiogenesis, such as vascular endothelial growth factor (VEGF), the antibodies restrict the blood supply to tumours, impeding their growth.
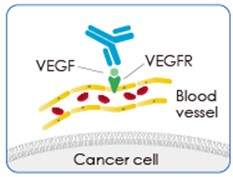
Example:
Bevacizumab (Avastin®): Targets vascular endothelial growth factor (VEGF), inhibiting the formation of new blood vessels that supply tumours. It is used for several types of cancer, including colorectal, lung, and ovarian cancer.
6. Drug conjugation
Monoclonal antibody drugs can be conjugated with chemotherapy drugs or radioactive particles. This approach allows for targeted delivery of the drug directly to cancer cells, maximising its efficacy while minimising systemic toxicity.
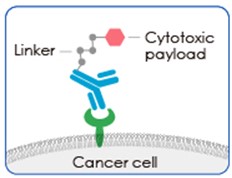
Example:
Brentuximab vedotin (Adcetris®): Combines an anti-CD30 antibody with a chemotherapy drug. It specifically delivers the chemotherapy to CD30-positive lymphomas, maximising its effectiveness.
7. Bispecific antibodies
Advances in engineering have enabled the development of bispecific antibodies that can simultaneously bind to multiple targets. These antibodies can engage both cancer cells and immune cells, enhancing immune cell activation and targeting cancer cells more effectively.
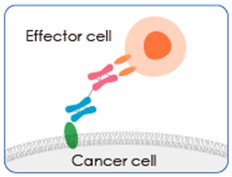
Example:
Blinatumomab (Blincyto®): Engages both CD19 on B cells and CD3 on T cells, bringing them together to eliminate cancer cells. It is used for acute lymphoblastic leukaemia.
Zahavi et al., (2020)
Liu et al., (2022)
Global Approved Bispecific Antibodies
| Drug Name | Trade Name | Company | Targets | First Approved Date (Country) | Indications |
|---|---|---|---|---|---|
| Catumaxomab | Removab | Trion Pharma | CD20/EpCAM | 2009 (withdrawn in 2017) | Malignant ascites |
| Blinatumomab | Blincyto | Amgen | CD3/CD19 | Dec 2014 (USA) | Relapsed or refractory precursor B-cell acute lymphoblastic leukaemia (ALL) |
| Amivantamab-vmjw | Rybrevant | Janssen | EGFR/cMet | May 2021 (USA) | Non-small cell lung cancer |
| Tebentafusp-tebn | Kimmtrak | Immunocore | GP100/CD3 | Jan 2022 (USA) | Unresectable or metastatic uveal melanoma |
| Cadonilimab | 开坦尼® | Akeso, Inc. | PD-1/CTLA-4 | Jun 2022 (China) | Cervical cancer |
| Mosunetuzumab | Lunsumio | Roche | CD20/CD3 | Jun 2022 (EU) | Relapsed or refractory (R/R) follicular lymphoma (FL) |
| Teclistamab | Tecvayli | Janssen | BCMA/CD3 | Aug 2022 (EU) | Relapsed and refractory multiple myeloma |
| Glofitamab | COLUMVI | Roche Canada | CD3/CD20 | Mar 2023 (Canada) | Diffuse large B cell lymphoma (DLBCL) |
| Epcoritamab | Epkinly | Genmab US | CD3/CD20 | May 2023 (USA) | Diffuse large B cell lymphoma (DLBCL) |
Esfandiari et al., (2022)
Benefits:
- Targeted therapy: Monoclonal antibody drugs specifically bind to cancer cells, selectively destroying or inhibiting their growth while sparing healthy cells.
- Reduced side effects: Monoclonal antibody drugs have fewer adverse effects compared to traditional chemotherapy, as they minimise harm to healthy cells.
- Enhanced efficacy: Monoclonal antibody drugs can be designed to carry out various functions, such as blocking the growth of blood vessels that supply tumours or activating the immune system to improve treatment effectiveness.
- Combination therapies: Monoclonal antibody drugs can be used in combination with other cancer treatments, such as chemotherapy or radiation therapy to synergistically enhance response rates.
- Personalised medicine: Monoclonal antibody drugs can be customised to target specific molecular characteristics of individual patients’ tumours.
- Expanded treatment options: Monoclonal antibody drugs have broadened the range of available treatments for different types of cancer.
Limitations:
- Limited effectiveness in certain cancer types: Monoclonal antibody drugs may not be effective against all types of cancer. The success of these drugs can vary depending on the specific molecular targets present in different cancer cells.
- Development of resistance: Over time, cancer cells can develop resistance to monoclonal antibody drugs, reducing their effectiveness. This resistance can arise through various mechanisms, such as alterations in the target molecules or activation of alternative signalling pathways.
- High cost: Monoclonal antibody drugs can be expensive, making them less accessible to some patients. The cost of production, development, and extensive clinical trials contributes to the high price of these therapies.
- Potential side effects: While monoclonal antibody drugs generally have fewer side effects compared to traditional chemotherapy, they can still cause adverse reactions in some individuals. These can include infusion reactions, allergic responses, or immune-related side effects, depending on the specific drug and patient.
- Limited penetration into solid tumours: Monoclonal antibody drugs may face challenges in penetrating deeply into solid tumours due to their large size. This can restrict their effectiveness in reaching all cancer cells within the tumour mass.
Abnova Products:
Information provided by Abnova.
Caltag Medsystems is the distributor of Abnova products in the UK and Ireland. If you have any questions about these products, please contact us.
